Colorectal Cancer Awareness Month 2023
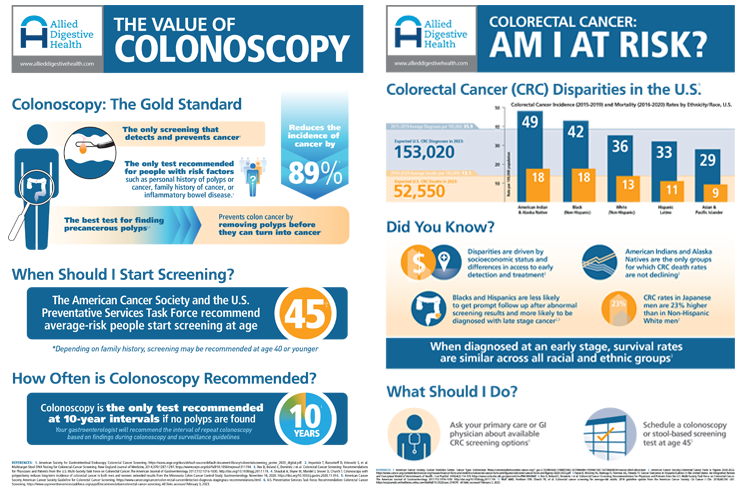
Watch this video on how a “Colonoscopy Screening is the only test
that both detects and removes precancerous polyps.”
What Is Colorectal Cancer?
Colorectal cancer is the third leading cause of cancer death in the United States, often because it is not detected early enough. Colorectal cancer refers to cancer in the colon (large intestine) and rectum. It is sometimes used interchangeably with the terms “colon cancer” or “rectal cancer.” Colorectal cancer typically begins in the form of noncancerous polyps, which turn into cancerous polyps over time. Like other forms of cancer, colon cancer can metastasize, spreading to other areas of the body. Not all polyps in the colon and rectum become cancerous, but they are often removed as a preventative measure.
Am I At Risk for Colorectal Cancer?
The American Cancer Society, US Preventive Services Task Force and US Multisociety Task Force for Colorectal Cancer have all recommended that the threshold for colon cancer testing be lowered from age 50 to 45. Some of the risk factors that increase one’s chance for colorectal cancer include a family history of colon polyps or cancer, or other types of cancers, type 2 diabetes, being of Ashkenazi Jewish descent, being of African American descent, obesity, inflammatory bowel disease (IBD), alcohol abuse, cigarette smoking, a sedentary lifestyle, red meat consumption (particularly in women), and consuming meat at high temperatures.
Sharing your family history with your physician is crucial when it comes to early detection of colon cancer. While the current recommendation is you should be screened at age 45, you may be able to have a screening earlier if you have high risk factors, such as a family history of colon cancer or personal history of gastrointestinal disorders such as IBD.
What Are the Symptoms of Colorectal Cancer?
Colon cancer is diagnosed in stages, from stage 0 through stage IV. Unfortunately, by the time many patients experience symptoms, colon cancer has progressed to the later stages. Symptoms of colorectal cancer include:
- Sudden weight loss
- Unexplained fatigue
- Nausea and vomiting
- Diarrhea or constipation
- Blood in the stool
- Gas or stomach cramping
Unfortunately, these symptoms can mimic minor conditions, so they may often go ignored. You should report blood in the stool or any other changes in bowel movements, as it may not be colon cancer but may be indicative of a different gastrointestinal issue.
Is It Possible to Prevent Colon Cancer?
The best way to prevent colorectal cancer is to get screened for it.
While genetics do play a prominent role in the development of colon cancer, there are some preventative measures you can take to try to prevent colorectal cancer. Avoiding red meat, drinking alcohol moderately or not at all, and quitting cigarettes all can lower your risk of developing polyps and colon cancer. It’s also important to eat a balanced diet and exercise regularly, as obesity and a sedentary lifestyle are both risk factors for colorectal cancer.
How Can I Be Screened for Colorectal Cancer?
The gold standard when it comes to screening for colorectal cancer is colonoscopy. This is an outpatient procedure done under partial or full anesthesia, and most patients can resume work or normal activities soon after the test.
A colonoscopy looks for any abnormalities of the digestive tract. Your gastroenterologist will insert a long, thin tube into the anus to look for polyps or other abnormalities. Your physician may take tissue samples from the colon or rectum to be evaluated. If your doctor finds polyps during the screening, they can remove them during the procedure. Most polyps are “pre-cancerous”. Pre-cancerous polyps are themselves not cancerous, but have the potential to become one if they are not removed in time. This is how colonoscopy is the best and most effective tool in preventing colorectal cancer – it can remove polyps before they can turn into cancer.
Other methods to screen for colorectal cancer include flexible sigmoidoscopy, CT colonography, or stool based testing. Stool based testing are looking for occult blood or abnormal DNA that could suggest the presence of colorectal cancer. While such testing can be effective in detecting colorectal cancer, they are not as effective as colonoscopy in detecting colon polyps and thus preventing one from getting colorectal cancer.
What Are the Stages of Colorectal Cancer?
Colorectal and colon cancer are divided into four stages, with substages. The gastroenterologist determines the stage of the cancer by the size of the tumor, if the cancer has spread to nearby lymph nodes, and if the cancer has spread to primary organs (such as the lungs or liver).
- Stage 0: This is the earliest stage, also known as carcinoma in situ. The cancer has not grown beyond the innermost lining of the colon or rectum (mucosa layer).
- Stage I: This cancer has spread through the muscularis mucosa into the submucosa, but is still in an early stage, and has not left the colon or the rectal area.
- Stage II: Stage two has several substages. In stage II, the cancer has spread beyond the colon but has not yet reached nearby lymph nodes or vital organs.
- Stage III: Stage three also has several substages. During this stage of colon cancer, the cancer has spread to nearby lymph nodes but has not spread to vital organs.
- Stage IV: Stage four is the most serious type of colon cancer. During this stage, it is likely that the cancer will metastasize and spread to vital organs.
Early detection of colon cancer is exceedingly imperative. The five-year survival rate for stage II colon cancer is 72 percent, while the five-year survival rate for stage IV colorectal cancer is 16 percent. If colonoscopy detects colorectal cancer in earlier stages, the chances of survival are much higher.
What Is the Treatment for Colon Cancer?
The treatment for colorectal cancer depends on the stage it is in, the location of the cancer, and if it has spread to vital organs. The most common treatment for colorectal cancer is the removal of the cancer itself via surgery. Other treatments can include radiofrequency ablation (RFA) or cryoablation, radiation, chemotherapy, and targeted therapies, such as anti-angiogenesis therapy, immunotherapy, and epidermal growth factor receptor (EGFR) inhibitors.
Footer
©2025 Allied Digestive Health. All Rights Reserved.